18:23 26th April 2021 | Male Fertility
Infertility is defined as the inability of a couple to conceive after one year of unprotected, penetrative sexual intercourse. Infertility affects 10% of couples worldwide and is a major cause of marital disharmony, depression and even stigma in Sub- Saharan Africa.
In this part of the world, more emphasis is laid on the female partner as the culprit in the challenge of fertility. However, the crucial factor of male infertility is on the rise and is a vital contributor to the prevalence of infertility.
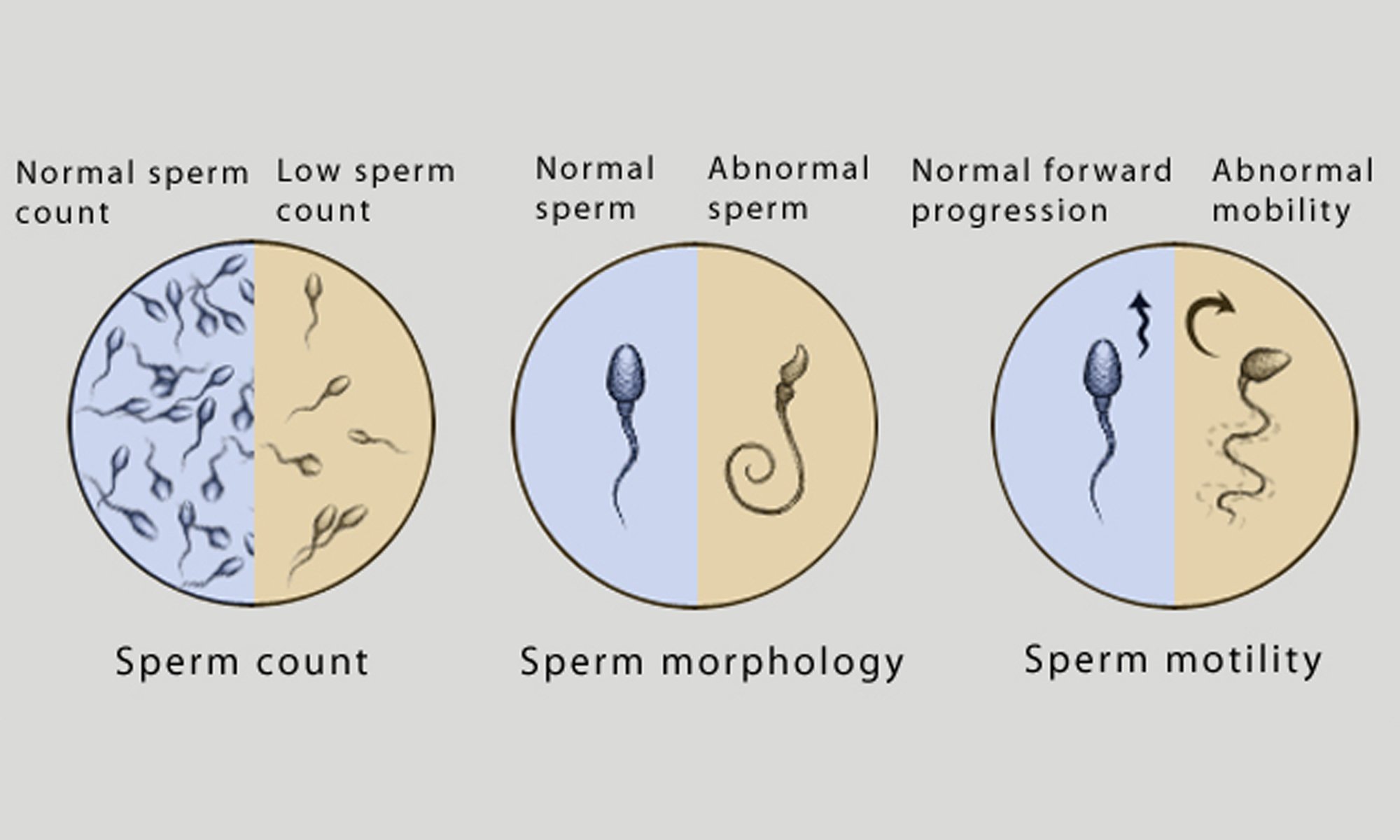
30% of cases of infertility are due to male factor, 30% due to female factor, 30% due to combined male and female factors and about 5-10% of cases are unexplained. Male factor infertility contributes to about 30- 50% of infertility cases. The spectrum of male infertility varies from low sperm count (oligospermia), low motility (asthenospermia), low normal forms (teratospermia), combined disorders to complete absence of sperm cells (azoospermia). These can only be discovered during routine seminal fluid analysis. Other conditions include erectile dysfunction that can present with either retrograde ejaculation (dry orgasm) in which sperm is seen in the urine rather than in the semen due to various conditions
Evaluation of infertility leads to the discovery of any of these diagnostic challenges. The question is asked often, “Why is male infertility on the rise?” Firstly, we need to identify the possible causes of male infertility.
Idiopathic: This means it is possible to have any of these conditions without any underlying identifiable cause.
Genetic: There could also be genetic causes that could be inherited from the father. e.g., Chromosomal disorders like Klinefelter syndrome are the commonest genetic cause of absent sperms in the semen(azoospermia) and in this condition, men would present with tall stature, enlarged breasts(gynaecomastia), very small testicles (testicular atrophy) and absent sperm cells. Other genetic conditions include genetic deletions of what we refer to as the ‘Y’ chromosome. Congenital absence of male reproductive structures e.g., spermatic cords. The list is not exhaustive.
Infections: Complications of infections such as Chlamydia and Gonorrhea can lead to obstruction in the pathway of sperm from the point of production to the point of ejaculation. This condition is referred to as obstructive azoospermia. Other infections like childhood mumps orchitis can predispose to male infertility. Undescended testicles is another condition that is noteworthy.
Lifestyle/environmental: Factors such as smoking and alcohol have been shown to adversely affect sperm parameters and contribute significantly to male infertility. Quitting smoking and alcohol abuse are modifiable risk factors for infertility.
Medical conditions: like diabetes mellitus and cancers also contribute to male infertility
Medical therapy: The use of cytotoxic drugs for cancer treatments and radiation therapy can affect sperm production by causing damage to testicular cells. An innovation to help such men is to freeze their sperms before undergoing such treatments.
Acquired: Cases of trauma to the testicles from road traffic accidents or falls are factors.
Evaluation of male infertility involves taking adequate history by the fertility specialist to ascertain possible causes and further evaluate by doing seminal fluid analysis, hormonal evaluation and sometimes genetic testing.
Hope is not lost when male infertility is diagnosed.
The concept of assisted reproductive technology through IVF (In vitro fertilization)/ ICSI (Intracytoplasmic sperm injection) has revolutionized fertility practice. Intracytoplasmic sperm injection means the injection of an individual sperm cell into an egg with the objective of generating embryos that would be transferred into a woman to achieve conception. With the advent of IVF/ICSI, it is now possible to help couples achieve conception with very poor semen parameters. In cases of azoospermia (absent sperm cells), various surgical techniques to retrieve sperm cells directly from the testes are now available which are readily used such as PESA (Percutaneous Epididymal Sperm Aspiration), TESA (Testicular Sperm Aspiration) and TESE (Testicular Sperm Extraction). This has brought hope to many men who may have given up on their journey to becoming a genetic father.
Our free attendance forums are a great opportunity to speak to our fertility specialists and counsellors about overcoming conception challenges. Join us https://www.thebridgeclinic.com/patient-care/promotions-campaigns/welcome-forum to find out more.
By Dr. Babatunde Ogunniran M.B.B.S, FMCOG, Consultant Gynaecologist
To find out about how Bridge Clinic can assist you, contact Nigeria’s most trusted fertility centre today.
Email: enquiries@thebridgeclinic.com
Call: 01 631 0092 / Whatsapp: +234 (0)810 460 7791.
Visit: 66 Oduduwa Way, Ikeja GRA
Search by condition, treatment or keyword and conveniently browse our informative articles
Book an appointment online or search for a clinic close to you.
Book an Appointment