13:02 10th June 2019 | IVF
In Nigeria and most of sub-saharan Africa, a high premium is placed on child bearing. Studies have reported rates of infertility as high as 40% of women who have completed their reproductive years without bearing a child ( 12 ) . National Health Statistics Report from the U.S has results that the percentage of married women aged 15 – 44 who were infertile fell from 8.4% in 1982 (2.4million women) to 6% (1.5million) in 2006 – 2010. ( 13 ). However, the incidence of infertility is still very high due to several factors. With the advent of assisted reproductive techniques, a lot of couples who hitherto would have remained childless have the chance of carrying children of their own. The process of In-vitro fertilization (IVF) involves gamete retrieval from both male and female partners, ensuring fertilization and culture of the generated embryos. The process culminates in embryo transfer where viable embryos are carefully transferred back to the uterus of the woman with the hope of implantation and pregnancy.
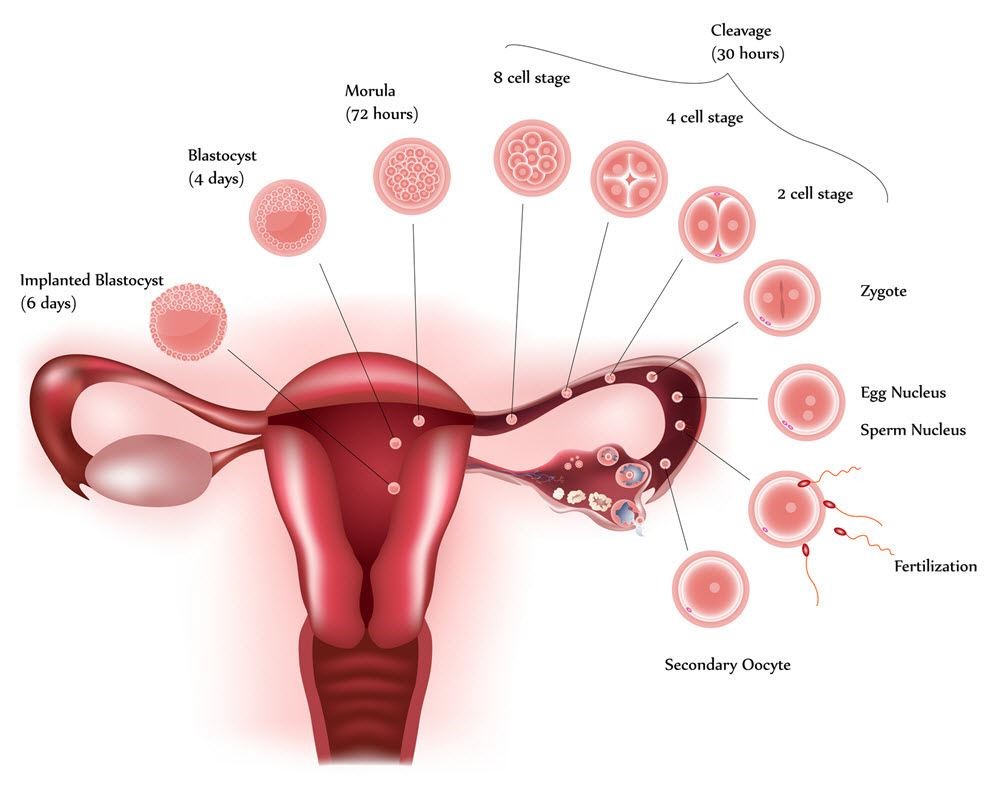
Implantation
This is the attachment of one or more embryos (blastocyst stage or day 3 cleavage stage) to the endometrial lining of the uterus, leading to further development into a baby(ies). It occurs following both natural and IVF cycles.
Before IVF treatment is recommended, a full history is taken and the couple are examined by the treating physician. Baseline hormonal laboratory investigations, ultrasound scans as well as semen analysis are done. The baseline hormonal check are early follicular phase serum FSH – follicle stimulating hormone, LH – Luteinizing hormone , prolactin, DHEAS – Dehydroepiandrosterone- sulfate and estradiol levels . These and other factors such as age, Antral follicular count and body mass index are considered in choosing a suitable stimulation protocol for the IVF treatment. A good ‘down regulation’ is important where the physician takes control of the cycle – Buserelin injections- the aim is to achieve a thin endometrial lining < 4mm. When this has been achieved, the next in line is the ovarian stimulation - typically involves daily injections of Follicle stimulating hormone which is followed by oocyte retrieval and the same day sperm is collected from the male partner. These gametes are fertilized either by conventional IVF, ICSI or IMSI resulting in fertilization. The resulting embryos are then cultured in the incubator for 3 to 5 days with the aim of transferring top quality blastocysts back into the uterus when suitable hoping for successful implantation.
Repeated implantation failure
Occurs when a woman undergoes three or more failed IVF attempts (with good quality embryos) or when more than 10 top grade embryos have been transferred into the client’s uterus over many cycles with no success. Looking at the process flow and management of clients in the IVF clinic, some of the factors that could affect implantation are embryo quality, uterine receptivity, and embryo transfer technique/skill of the physician, infection, stress and the presence of natural killer cells antibody in the woman.
Embryo quality
This is related to the quality of the egg and the quality of the sperm. Advancing age in the woman negatively impacts her egg quality. Eggs from older women are more prone to chromosomal defects such as aneuploidies (presence of wrong number of chromosomes.
Sperm quality is determined by genetic factors, male lifestyle choices such as smoking and excessive alcohol intake. Environmental pollutants can also have a negative impact on the sperm. With the advent of comprehensive chromosome screening, it is now possible to screen all 24 chromosomes (22 autosomes and 2 sex chromosomes) for the presence of aneuploidy (even though the effectiveness of such a technique to increase live birth via Assisted Reproductive Technologies in clinical practice is still not proven). Chromosome abnormalities identified by comparative genomic hybridization in embryos from women with repeated implantation failure. (14)
Uterine receptivity
This Is influenced by the endometrial thickness and hormone levels. An endometrial thickness between 8 – 15mm is favorable for implantation. The type of protocol used for the cycle is determined individually. The short protocols are milder and usually are used for clients who are presumed ‘poor responders’ by the selection criteria of – Age, BMI and laboratory investigations of the hormonals and possible previous stimulation outcome.
Presence of high levels of the estrogen in the body during a fresh embryo transfer can negatively affect uterine receptivity. Other factors that can affect uterine receptivity is the type of protocol used; commonly used protocols are long, short and antagonist. It is advisable that the antagonist protocol be followed by cryopreservation of all embryos with the client coming back for frozen embryo transfer; as the rate of implantation following this protocol is usually lower.
Another important factor that can affect implantation is the appearance of the endometrial lining. Presence of adhesions, polyps or fibroids within the cavity, adenomyosis, anatomical defects. The presence of all the factors mentioned above can negatively affect implantation.
Endometrial receptivity is assessed during IVF, with the help of ultrasound images via 2D or 3D scan machines. Endometrial assessment starts from down regulation scans where the endometrium is expected to thin out after a menstrual bleed. In the same vein, an endometrium of greater than 8mm, which is trilaminar, is believed to be optimum for embryo transfer.
It is a well-known fact that the endometrium becomes receptive only after progesterone exposure. Progesterone brings about necessary changes in endometrium (converts the endometrium from proliferative to secretory phase) so that it becomes ready to accept the embryo. Recently, some successes have been seen with frozen embryo transfers than fresh embryo transfers. It is hypothesized that high estrogen concentration in the body during the fresh IVF cycle compromises endometrial receptivity.
Embryo transfer
The skill of the physician can impact implantation and pregnancy. The approach or the method used by the physician is very key to the outcome of the procedure. Having blood free embryo transfer has been shown to favour implantation. In some cases removing cervical mucus by aspiration before transfer of the embryos can lead to successful pregnancy outcome.` Dropping’ of the embryos at the right depth and as gentle as possible so as not to cause uterine contractions is important for the success of the transfer.
Blood staining the tip of the embryo transfer catheter negatively affects pregnancy rate. The blood stained tip also signifies that the process of transfer was traumatic, and this is what should be avoided during transfer. It should be as gentle and atraumatic as possible.
Infection has also been named with this condition, Recurrent Implantation failure. Bacterial colonization from chronic endometriosis often with no clinical signs of infection presents with bacterial in the endometrium which leads to abnormal lymphocyte counts and as a result, an environment is created that interrupts normal endometrial receptivity. Findings of implantation rates of those cured of infection was 37% compared to those not cured which was 17%. However live birth rates with the next cycle after infection was cured, was significant with a rate of 61% in comparison to 13% in those that could not be cured with antibiotics
Natural Killer (NK) cells: Some women with recurrent implantation failure have been shown to have higher NK cells and preconception natural killer cells.
Conclusion: Implantation failure is a complex problem with a wide variety of aetiologies and mechanisms as well as treatment options.
Recommendation: This would vary depending on the problem. Each client’s care will be tailored to meet the needs depending on the unique set of characteristics. There is not one treatment option but many depending on aetiology of the problem. The use of antibiotics, vasoprin for increased blood flow to the uterus and supportive treatment (counselling, encouraging the clients to have a more enjoyable and conducive environment) will go a long way in helping to increase implantation and hence pregnancy rates.
References:
Search by condition, treatment or keyword and conveniently browse our informative articles
Book an appointment online or search for a clinic close to you.
Book an Appointment