17:47 2nd September 2019 | PCOS
Polycystic ovary syndrome (PCOS) is a hormonal disorder common among women of reproductive age. Women with PCOS may have infrequent or prolonged menstrual periods or excess male hormone (androgen) levels. The ovaries may develop numerous small collections of fluid (follicles) and fail to regularly release eggs.
The exact cause of PCOS is unknown. Early diagnosis and treatment along with weight loss may reduce the risk of long-term complications such as type 2 diabetes and heart disease.
Signs and symptoms of PCOS may develop around the time of the first menstrual period during puberty. Sometimes PCOS develops later, for example, in response to substantial weight gain. Signs and symptoms of PCOS vary but are typically more severe if you're obese.
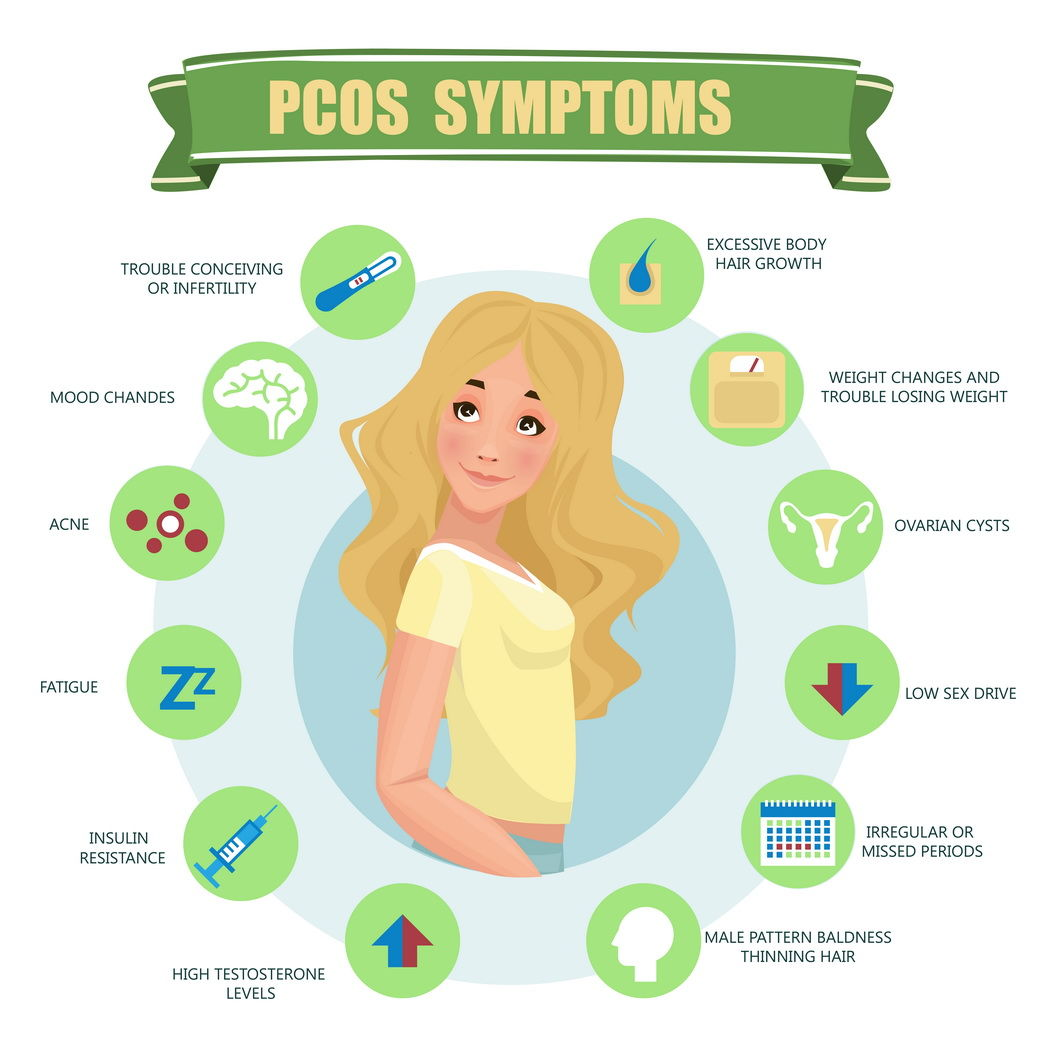
A diagnosis of PCOS is made when you experience at least two of these signs:
• Irregular Periods. Infrequent, irregular or prolonged menstrual cycles are the most common sign of PCOS. For example, you might have fewer than nine periods a year, more than 35 days between periods and abnormally heavy periods.
• Excess Androgen. Elevated levels of male hormone may result in physical signs, such as excess facial and body hair (hirsutism), and occasionally severe acne and male-pattern baldness.
• Polycystic Ovaries. One’s ovaries might be enlarged and contain follicles that surround the eggs. As a result, the ovaries might fail to function regularly.
The exact cause of PCOS isn't known. Factors that might play a role include:
• Excess Insulin. Insulin is the hormone produced in the pancreas that allows cells to use sugar, one’s body's primary energy supply. If one’s cells become resistant to the action of insulin, then one’s blood sugar levels can rise and one’s body might produce more insulin. Excess insulin might increase androgen production, causing difficulty with ovulation.
• Low-grade Inflammation. This term is used to describe white blood cells' production of substances to fight infection. Research has shown that women with PCOS have a type of low-grade inflammation that stimulates polycystic ovaries to produce androgens, which can lead to heart and blood vessel problems.
• Heredity. Research suggests that certain genes might be linked to PCOS.
• Excess Androgen. The ovaries produce abnormally high levels of androgen, resulting in hirsutism and acne.
Complications of PCOS can include:
• Infertility
• Gestational diabetes or pregnancy-induced high blood pressure
• Miscarriage or premature birth
• Nonalcoholic steatohepatitis — a severe liver inflammation caused by fat accumulation in the liver
• Metabolic syndrome — a cluster of conditions including high blood pressure, high blood sugar, and abnormal cholesterol or triglyceride levels that significantly increase one’s risk of cardiovascular disease
• Type 2 diabetes or prediabetes
• Sleep apnea
• Depression, anxiety and eating disorders
• Abnormal uterine bleeding
• Cancer of the uterine lining (endometrial cancer)
• Obesity is associated with PCOS and can worsen complications of the disorder.
Firstly, if women have irregular periods, they should keep a diary. The diary should clearly note the days when they start menstruation and when they finish, and this diary should be kept for 6 to 12 months. This record will be useful when an appointment is made with the specialist. The diary may show that although periods are not happening every 4 weeks, they may be coming every 5 to 6 weeks, which may be normal in that age group, especially for girls under 18.
Secondly, should young adults be referred for a pelvic ultrasound scan to make a diagnosis of PCO? Most recently, International Guidelines on PCO recommended that “the diagnosis of PCOS should not be made by ultrasound scan, at least before 8 years have elapsed from the start of menarche, the onset of periods”. So, if the period started at the age of 11, then an ultrasound scan should not be done until the age of 19 to make a diagnosis of PCO. That is very important because there is an overlap between the pubertal development, hormonal changes, and the maturing process of the Hypothalamus-Pituitary-Ovarian axis in early adolescent years which may be confused with the PCOS. It is the duty of the clinician to explain to the young women and their parents that their hormonal systems are still maturing.
Thirdly, girls and women with PCOS risks should exercise regularly and remain physically active.
Fourthly, they should monitor what they eat. Women should be encouraged to eat low-glycemic food with high vegetable and fruit content. The importance of that is that it reduces the risk of visceral obesity (fat deposition around the waist). It has been reported that the average waist size is getting bigger, and we see it every day. So, women can help themselves control their waist expansion by regular exercise. It has been noted that individuals who have a waist-hip ratio of greater more than 1, will potentially have a higher risk of developing other diseases in the long run such as diabetes and hypertension.
A healthy BMI is between 18.5 and 25. Once it is above 30, most of the manifestations of irregular cycles start, which then, of course, are considered to be the signs of PCOS.
Does bariatric surgery help with PCOS?
Bariatric surgery’s role in PCOS treatment is very limited. Bariatric surgery reduces the weight, but it also limits the absorption of healthy nutrients. It does lower the levels of free testosterone and it does increase the binding of free testosterone to the sex hormone-binding globulins. It will not have an immediate effect on hirsutism. Overall, there is a healthy trend of biochemical changes in the individual and if they have lost enough weight, their menstrual cycle’s pattern may improve significantly. However, it is not a cure for hirsutism and neither for PCOS.
Does homoeopathy cure PCOS?
There are no large-size studies to show the benefit as compared to traditional medicines used in regular practice. But there's no magic PCOS cure, no matter what the supporters of homoeopathy say.
Does yoga help in managing PCOS?
Yoga has positive benefits in improving morale and managing anxiety. It can help with coping mechanisms, and women can cope with their emotions and symptoms more positively, but yoga will not affect the natural history of PCOS or cure.
Has anyone ever cured PCOS completely?
Once the manifestations are there, it can’t be cured entirely. Only the signs of PCOS can be reduced in their intensity. For example, if a polycystic change has developed within the ovary, it will remain a polycystic ovary. But the manifestation becomes less obvious if you manage it proactively.
For example, if somebody has a BMI of 35 and they manage to lose weight proactively and their BMI becomes 25, then there is more than 80% chance their periods would become regular, there is a higher chance that their manifestations of acne will improve and they may not require any antibiotics or any hormonal manipulation. The intensity of hirsutism will also get better. But the change which has taken place within the ovary will remain there. So, it will still be diagnosed as polycystic ovary when an ultrasound scan will be carried out.
Have there been any recent advanced research in PCOS?
Firstly, science is moving in a direction to understand what is the best way of diagnosing it and treating various manifestations of PCOS. Secondly, science is moving towards a very focused approach on how to treat women with various manifestations, because some of them will have very little manifestations and they may have PCOS with cycle problems. So, that is a different group. Then, there is a group of women who have severe manifestations of the condition. The new focus is on a lifecycle approach and to encourage a healthy lifestyle. There is a huge group of experts believing in educating women rather than giving them a ton of hormones.
The role of laser treatment for hair growth is increasing rapidly and there is need to learn which type of laser is more specific for various types of hirsutism and what is the long-term impact of such treatments on hair re-growth.
PCOS can manifest itself with excessive loss of hair leading to generalized thinning of hair and baldness. More work is required on drugs which bind to free circulating androgens, local treatments, as well as the role of hair growth stimulants and anti-inflammatory agents.
And lastly, of course, bariatric surgery is coming into focus, which can help to control the weight of the women and give them a healthy lifestyle. Because when they’re overweight, their confidence level is low, they feel depressed, they can’t exercise because of the excessive weight constraints. When they lose weight, then certainly it is a stimulus for them.
Finally, we must invest more to understand what women want and think about their condition, its impact on them. And we know now, there is a big psychological impact on women, on their morale, on their energy level, and their anxiety level. So, more and more input is coming from the psychiatrists and psychologists who can try to understand how to support women, rather than find a magic PCOS cure.
What advice would you give to people who have PCOS and those who suspect something, but are afraid to be diagnosed with PCOS?
It is important to encourage women not to be afraid of asking their physicians difficult questions during the examinations and visits, and they should have a realistic discussion and expectations. A realistic discussion is talking about what one’s symptoms are, what tests you need and what one’s precise diagnosis is.
And the expectation is that sometimes the doctor may not know answers to all the questions. Each woman needs to find an appropriate specialist, who can look after them, and be patient because in PCOS there is no magic cure. It is a lifelong condition, but it is not cancer and neither is it a disease, it is a syndrome manifesting in different ways with different symptoms. And every condition has to be managed and they should work very closely with their physician.
We should emphasize the following: junk food is not good for you! Enrich one’s diet with low-glycemic index and rich in antioxidants — more nuts, more fruit and vegetables. They can help themselves rather expecting physicians to help them with medication.
To find out about how Bridge Clinic can assist you, contact Nigeria’s most fertile fertility clinic today.
Email: enquiries@thebridgeclinic.com
Call: 01 631 0092 / Whatsapp: +234 (0)810 460 7791.
Visit: 66 Oduduwa Way, Ikeja GRA
Search by condition, treatment or keyword and conveniently browse our informative articles
Book an appointment online or search for a clinic close to you.
Book an Appointment